INTRAMAMMARY LYMPH NODES
BIRADS 2 FINDINGS
There are numerous lesions that develop in the breast that are not breast cancer and do not become cancer such as cysts and fibroadenomas. One of the important aspects of interpreting mammography screening studies is being able to identify findings on the study that do not represent breast cancer and do not need the patient to be recalled for additional evaluation. Among these are intramammary lymph nodes. We described intramammary lymph nodes, found on mammograms, in 1982 ¹. I am not aware of any embryological studies that track the development off the lymphatic system and nodal development, but since the breast develops as a “skin gland” on the upper chest wall, and breast tissue commonly extends up into the axilla, it is it is likely, and not surprising that lymph nodes, commonly seen in the axilla, extend down into the upper outer portion of the breast.
Intramammary lymph nodes are seen, mammographically, in approximately 5% of women. They appear at the edge of the parenchymal cone of the breast, toward the periphery near the junction of the subcutaneous fat and the parenchyma ². I have only seen one that was more than 2/3 of the way to the nipple. They are also almost all above the axis of the nipple.

Pathologists claim to have found lymph nodes in all quadrants of the breast, but the lymph nodes evident by mammography are almost (if not) all in the lateral half of the breast. To my knowledge there has been only one paper that presented two cases of intramammary lymph nodes evident by mammogrpahy in the medial breast, but these were described as “lymphoid tissue” and an actual “node” was not described ³.
The diagnosis is safely made for a structure in the lateral half of the breast toward its periphery that is sharply defined, perhaps slightly lobulated, 1 cm or smaller in size, and “reniform” in shape. This shape is due to the fatty hilum of the node that is often seen as a radiolucent center when the node is seen “en face”.
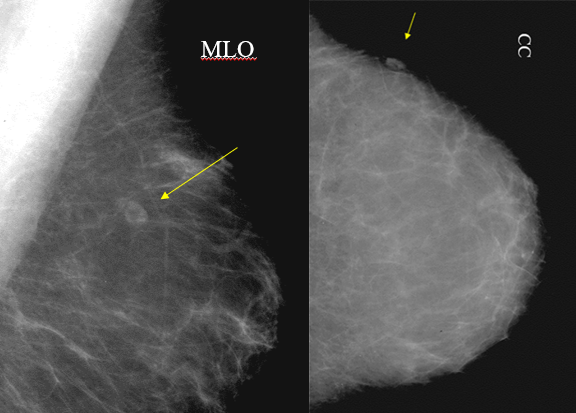
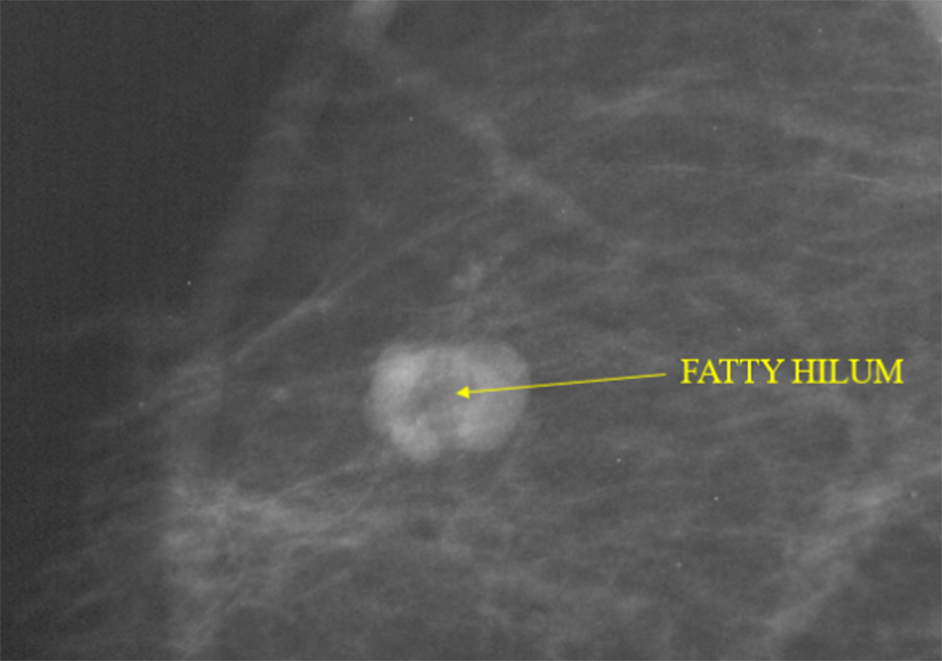
The sharp margins and reniform shape are the most important criteria. Fat in the hilum increases the certainty. When these criteria are present, then no further investigation is needed.
The presence of intramammary lymph nodes is so common, that a BIRADS 2 classification may not be needed unless there is concern that someone with less experience might misinterpret the node and a BIRADS 2 identification will clarify its benign nature.
LOCATION IS IMPORTANT
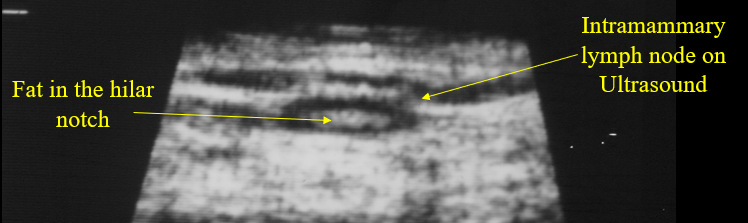
The interpretation of an intramammary lymph node should not be made when a mass is seen in any other section of the breast unless the lesion has a clearly defined lucent hilum. Since not all upper-outer quadrant masses are benign lymph nodes, if the lesion does not have the morphological characteristics of a benign intramammary lymph node, including a renifrorm shape or a lucent hilar notch and smooth, sharply defined margins, an upper-outer-quadrant lesion should arouse suspicion. If the morphology is not clear, magnification mammography may better demonstrate the shape and sharply defined margins. If this is not convincing, then ultrasound can be used to show the echogenic fat in the hilar notch.
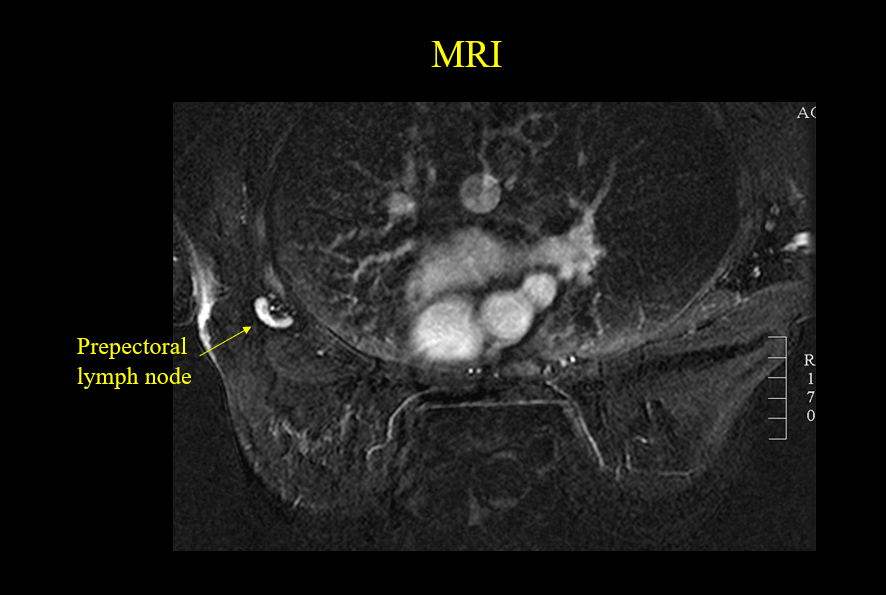
It is very unusual, but we have seen intramammary lymph nodes deep in the breast toward the center of the breast. These “prepectoral” lymph nodes can rarely be seen on mammograms and, on occasion, be seen on MRI.
METASTATIC DISEASE TO AN INTRAMAMMARY LYMPH NODE
Breast cancer can spread to intramammary lymph nodes. Intramammary lymph node involvement should be suspected when the node is larger than 1 cm and is round or oval without a hilum, and there is an associated breast malignancy ⁴.
We have seen benign enlargement of intramammary lymph nodes in women who have an associated dermatitis or mastitis. Without these other clear causes for nodal enlargement, biopsy is recommended for intramammary lymph nodes of 1 cm or greater that are round or oval and do not have a fatty hilum ⁵.
There still seems to be some debate about the clinical significance of metastatic disease involving an intramammary node. Some argue that it is the same as having axillary lymph node involvement ⁶ and predicts a poorer outcome ⁷, but others disagree⁸⁹¹⁰.
LYMPHOMA INVOLVING THE BREAST
Primary lymphoma can also involve intramammary lymph nodes. We published a paper that included five women whose primary lymphoma was in the breast and seven who had known lymphoma elsewhere with lesions in the breast as well. The abnormal mammographic findings varied from fairly discrete nodules to diffuse involvement of the parenchyma and skin¹¹.
CONCLUSIONS
Benign, intramammary lymph nodes are very common. If they are in the outer periphery of the breast (usually above the axis of the nipple, and are 1 cm. or smaller with sharply defined margins and a reinform shape with fat in the hilum, no further investigation is required.
REFERENCES
1.Meyer JE, Kopans DB. The radiographic appearance of normal intramammary lymph nodes. Breast 1982; 40:30-32.
2.Stomper PC, Leibowich 5, Meyer JE. The prevalence and distribution of well circumscribed nodules on screening mammography: analysis of 1500 mammograms. Breast Dis 1991:4:197-203 2. Gordon PB, Gilks B. Sonographic appearance of normal
3.Meyer JE, Ferraro FA, Frenna TH, et al. Mammographic appearance of normal intramammary lymph nodes in an atypical location. AJR Am J Roentgenol 1993;161:779–780
4.Günhan-Bilgen I, Memiş A, Ustün EE. Metastatic intramammary lymph nodes: mammographic and ultrasonographic features. Eur J Radiol. 2001 Oct;40(1):24-9. doi: 10.1016/s0720-048x(01)00373-4. PMID: 11673004.
5.Lindfors KK, Kopans DB, Googe PB, McCarthy KA, Koerner FC, Meyer JE. Breast cancer metastasis to intramammary lymph nodes. AJR Am J Roentgenol. 1986 Jan;146(1):133-6. doi: 10.2214/ajr.146.1.133. Erratum in: AJR Am J Roentgenol 1986 Mar;146(3):614. PMID: 3000154.
6.Lee S, K, Kim S, Choi M, -Y, Kim J, Lee J, Jung S, P, Choe J, -H, Kim J, -H, Kim J, S, Kil W, H, Lee J, E, Nam S, J: The Clinical Meaning of Intramammary Lymph Nodes. Oncology 2013;84:1-5. doi: 10.1159/000340016
7.Hogan BV, Peter MB, Shenoy H, Horgan K, Shaaban A. Intramammary lymph node metastasis predicts poorer survival in breast cancer patients. Surg Oncol. 2010 Mar;19(1):11-6. doi: 10.1016/j.suronc.2008.12.009. Epub 2009 Jan 26. PMID: 19171479.
8.Diaz R, Degnim AC, Boughey JC, Nassar A, Jakub JW. A positive intramammary lymph node does not mandate a complete axillary node dissection. Am J Surg. 2012 Feb;203(2):151-5. doi: 10.1016/j.amjsurg.2011.01.030. Epub 2011 Jul 23. PMID: 21788008.
9.Khoury T, Fang Y, Karabakhtsian R, Mokhtar Desouki M, Nayak A, Hanna M, Sanati S, Peng X, Yan L, Li X, Fadare O, Ambrosone C, Jabbour N, Gaudioso C. The clinical significance of metastatic breast carcinoma to intramammary lymph node. Breast J. 2020 Feb;26(2):197-205. doi: 10.1111/tbj.13636. Epub 2019 Oct 6. PMID: 31588665; PMCID: PMC7869654.
10.Guth AA, Mercado C, Roses DF, Hiotis K, Skinner K, Diflo T, Cangiarella J. Intramammary lymph nodes and breast cancer: a marker for disease severity, or just another lymph node? Am J Surg. 2006 Oct;192(4):502-5. doi: 10.1016/j.amjsurg.2006.05.011. PMID: 16978960.
11.Meyer JE, Kopans DB, Long JC. Mammographic appearance of malignant lymphoma of the breast. Radiology. 1980 Jun;135(3):623-6. doi: 10.1148/radiology.135.3.7384445. PMID: 7384445.


