A COMPUTERIZED REPORTING SYSTEM
Since the screening examination is the only time that an early cancer may be detected and a life saved, clearly, the most important component of a breast cancer screening program is having the best equipment to obtain the highest quality studies. The program needs highly skilled technologists who can obtain the best images possible, and highly skilled radiologists to interpret the studies. An integral part of the imaging “chain” is the reporting system. Reports need to be clear, concise and with sufficient detail to clearly define and highlight any problems. The report should conclude with a description of what, if anything, needs to be done next.
In the early years of screening, we dictated reports to be typed by transcriptionists. Not only were there issues with the transcriptionists not understanding what was being said, but the reports were often wordy, poorly organized, and confusing. Some practices used a simple check list – Negative or Needs Additional Evaluation. With that system, either the patient was to be told that everything was “fine”, or she was told that she needed to return for additional imaging. This very telegraphic technique is a problem if the patient returns and it is unclear why the radiologist who called her back was concerned. Furthermore, the telegraphic system is fairly useless for learning and improving over time since there are no details to which outcomes can be compared. Consequently, we developed a computer reporting system. It eliminated the problems. The same findings on a study were reported in the same way with the same words by every radiologist. Referring physicians had no problem understanding what the study showed and what should be done. A computer reporting system can, efficiently, collect fundamental data and use it to generate fairy detailed reports while providing clear advice as to what needs to be done next, and when saved in a data base the reports become the foundation for a program of continual improvement.
SINGLE SCREEN INPUT
A major factor in developing a computer reporting system is to make itas easy as possible to use while collecting as much important detail about the study as possible. The system needs to be efficient so that the radiologist spends most of the time looking at the images and very little time looking at the computer reporting screen. The unput for the report should be a single screen on the computer. The radiologist should not have to page through multiple screens to generate a report. We developed a single screen system:
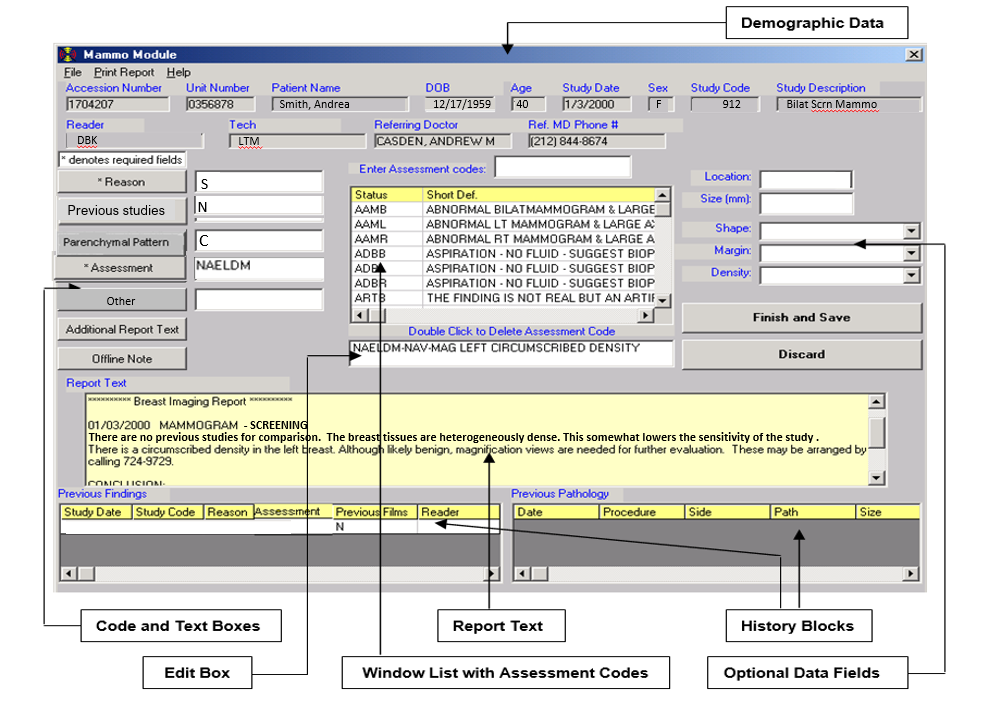
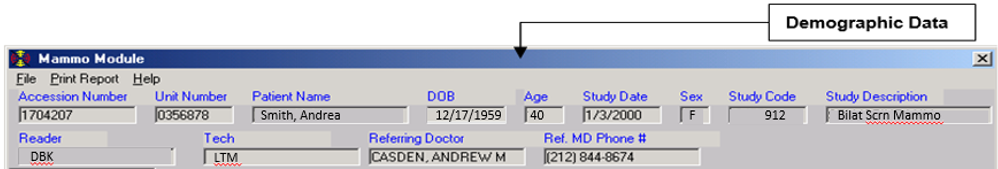
The top part of the screen is generated from the patient’s demographic information and is provided to the radiologist.
This next section is filled out using simple codes:
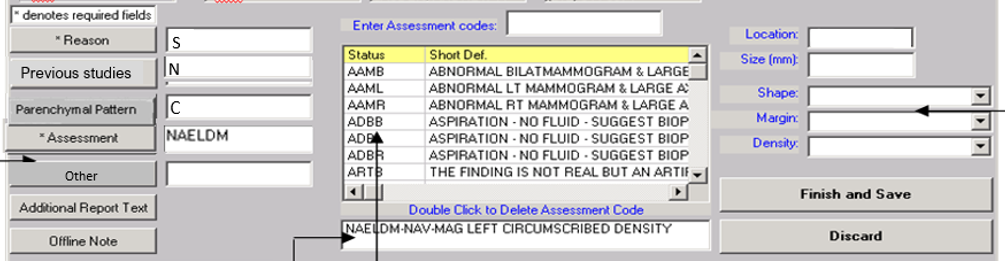
The blank boxes are filled in as needed by the radiologist. There are acceptable codes (and only acceptable codes) for each window.
REASON
We developed codes for virtually any reason for the study. Below are a sample – there are many more.
S = Screening
L = Patient has a lump
D = Patient has a discharge
R = Recall from screening
Etc.
PREVIOUS STUDIES
This field provides information in the report to explain whether other studies were used to evaluate the current study.
C= Comparison is made to the previous examinations.
N=There are no previous studies for comparison.
O=Comparison is made to outside examinations.
M=The previous studies are missing.
T=We are trying to obtain previous outside studies. If these can be obtained, they will be compared to the present examination and an addendum will be issued.
PARENCHYMAL PATTERNS (BIRADS TISSUE PATTERNS
This field provides information as to the sensitivity of the examination. The dense tissue patterns can obscure a lesion.
A: almost entirely fatty
B: scattered areas of fibroglandular density
C: heterogeneously dense – this somewhat lowers the sensitivity of mammography
D: extremely dense – this somewhat lowers the sensitivity of mammography
FINAL ASSESSMENT
Next, the “Assessment” code box receives the three to six-letter mnemonic codes, which cover virtually all breast imaging results. These are also available in the central box if the radiologist wants to scroll through to help the reader remember some of the codes. Simply typing or clicking the code(s) will insert appropriate descriptive phrases in both the edit box and report window.
If a code is entered that implies a “finding” then the appropriate optional data fields will open on the right.
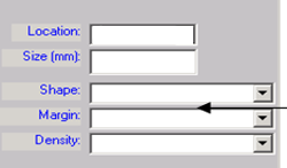
These allow for recording the location of the finding (simple codes), its size, shape, margins, and density (if it is a mass) (also simple codes), and the morphology and distribution of calcifications (also simple codes).
Based on the codes in the boxes, the appropriate full-text information appears immediately in the correct portion of the report. By returning to the assessment box, additional assessment codes may be entered to account for multiple findings when these are not covered by a single code. Again, the “findings” data fields will open for each subsequent assessment, and the information will be entered in the correct portion of the report. An erroneous code may be removed (thus removing all associated text) with a double mouse click in the edit box.
A FULL REPORT IS GENERATED
Based on these simple codes, a full report is constructed by the computer complete with a BIRADS final assessment.
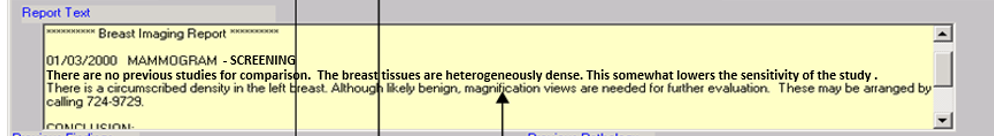
This full report will read:
“01/03/2000 MAMMOGRAM – SCREENING
There are no previous studies for comparison. The breast tissues are heterogeneously dense. This somewhat lowers the sensitivity of the study. There is a circumscribed mass in the left breast. Although likely benign, magnification views are recommended for further evaluation. These may be arranged by calling 617-724-9729
CONCLUSION:
Circumscribed density in the left breast. Additional evaluation is recommended.
BIRADS “0” Needs Additional Imaging”
ADDITIONAL INFORMATION
The bottom of the screen provides data on any previous studies and their results as well as previous pathology if the patient has had any previous biopsies. These are obtained from the Breast Imaging Database.
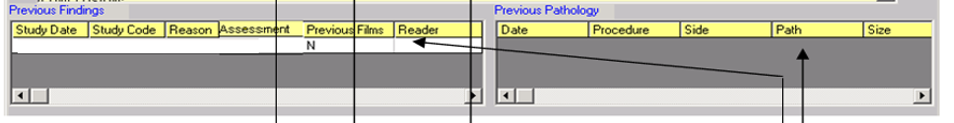
Thus, using a single screen, the important parts of the patient’s history are provided to the radiologist who can generate a complete report with as many details as needed with minimal interaction with the computer.


