AN OVERVIEW OF HOW TO SCREEN FOR BREAST CANCER
INTRODUCTION
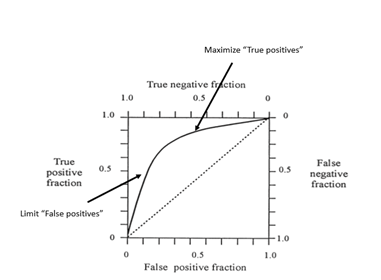
Figure 1
Even if both screening and diagnostic evaluations are being performed in the same facility it is much more efficient to have rooms and personnel dedicated to screening so that they do not get tied up with diagnostic studies that have unpredictable utilization times. Screening should be well organized so that women can be imaged soon after they arrive and can be on their way as soon as the study is completed with the whole sequence taking less than 30 minutes from the patient entering the screening unit to leaving.
In our system we scheduled 3-4 women an hour for each of our screening mammography units. gfWe have been doing DBT for years and the acquisition of screening DBT takes only a few seconds longer than FFDM. If the effort is well organized, a screening study (two projections of each breast) will take less than 5 minutes. However, it is important that women have a support iveand comfortable experience so that they will return each year. Consequently, we try to not place added pressure on the technologists so that they lose sight of their importance inreassuring our patients, and to not make our patients feel rushed. Ifhighly organized, and patients are prepared before entering the imaging space, screening can be done rapidly, but 4 patients per hour was our maximum.
GOWNED WAITING
To facilitate efficient care, once a woman is registered, she enters a changing area where she removes any clothing above the waist and puts on a paper (disposable) or cloth (launderable) gown, that will facilitate positioning for the mammogram. She then is seated in the private “gowned waiting area” that is separate from the facility’s general waiting area.
MAMMOGRPAHY ROOMS MUST BE UTILIZEDEFFICIENTLY
In order to maximize the screening of the large number of women needed to be screened each day, the mammography rooms need to be well managed. Each device must be disinfected between patients. Having digital units is much more efficient than the older screen/film (SF)systems. If SF is still being used then it may be facilitated by having the films processed by an assistant while the technologist manages the patients and the room. This is another reason why gowned waiting space is important. One patient may have had her images obtained and is returned to be seated in “gowned waiting” while the images are processed while a second screening patient is brought into the mammography room to have her images obtained. Certainly, with digital systems the process is expedited since the technologist can quickly review the images right in the room and discharge the patient rapidly if the images are of high quality.
TWO PROJECTIONS ARE BETTER THAN ONE
I strongly recommend that screening include the two basic projections – MLO and CC images of both breasts. Some countries do single view (MLO only)screening. This is faster, and less laboris required, but there is no question that cancers will be missed, and more women will be recalled for additional evaluation. In the UK they found that 2 view mammography detected 24% more cancers than single view MLO alone, and they also had a 15%lower recall rate ([3]). This was also true even when DBT is used for screening. There are cancers that are seen well on the CC projection using DBT, but are not seen on the MLO DBT images.
EQUIPMENT
There was a period of time when it was thought that resources could be saved by using basic, less expensive mammography units for screening. This was quickly shown to be a major mistake. The screening study is the only study that has the opportunity to save life by detecting breast cancers early. The failure of poor quality mammography ([4],[5])can best be seen in the failure of the Canadian National Breast Screening Studies (outliers among the RCT’s) to show any benefit from screening. It is clear that the screening test needs to be the highest quality possible to provide the optimum opportunity to detect cancers early.
HIGH QUALITY SCREENING MAMMOGRAMS ARECRITICAL
Since the screening study is the only chance for the patient to have her life saved, the screening mammogram needs to be the best that we can make it. Technologists who are performing the studies need to be well trained to obtain the best mammograms possible. The technologist needs to work with the patient so that she can pull the breast gently,but with some force, into the proper position to image as much of the tissuesas possible. It is simple to image the front of the breast, but imaging the back of the breast along the chest wall (a huge volume of tissue) takes training and experience. Breast cancers can develop in any part of the breast so that the technologist must work closely with the patient to get as close to the chest wall as possible. The mediolateral oblique (MLO) is the best position to maximize imaging the breast. A large percentage of cancers develop in the upper outer quadrant so imaging these tissues is critical for mammography screening.
The craniocaudal images complement the MLO. The breast should be elevated to, once again, permit imaging as far back as possible.
Compression is used in both projections to spread the structures apart; make the breast more uniform to permit optimal exposure; reduce scatter; reduce the amount of radiation needed; reduce motionblur; and hold the breast close to and over the detector. However, excessive compression is of no valueand only a cause for discomfort. The breast should be compressed until the free skin is “taut”. Beyond that has no value. If the patient complains of pain the technologist should reduce the compression and be certain that the system is not pinching the skin. She should work with the patient to try to achieve “taut” compression. If a patient has a bad experience she may notreturn for future screening and the benefits of screening will be lost. It is critical that the technologist strive to position the breast to maximize the tissues imaged while working to keep the patient as comfortable as possible. “Working with the patient” and involving her in the process is key to a successful study and having the patient return in the future.
INTERPRETING SCREENING MAMMOGRAMS
Once the technologist has obtained the images, they should be evaluated to be certain that they are of high quality. Has the positing been optimized to image as much of the breast as possible? There should be no motion. The structures need to be separated to try to avoid cancers being hidden by normal tissue. The breasts should have beenpositioned symmetrically so that the radiologist can appreciate any areas of asymmetry. If the images are high quality, then the technologist can send them on for inter pretation and the patient can put her clothes back on and leave the facility.
READING IN BATCHES
There have been numerous approaches to the interpretation of screening mammograms over the years. In an effort to reduce the anxiety that some women have waiting for their results, and to avoid having to recall women for diagnostic evaluation, efforts have been made to interpret screening studies,”online”, before women leave the screening facility and to also provide diagnostic evaluation if something is seen. Irecognize the convenience and reduction in anxiety that “immediate reads”provide, but I have also seen the risks. There is no question that cancers are missed when studies are interpreted too quickly and when the radiologist rushes the interpretation. If women have to wait for the interpretation, many become anxious and have other appointments, and they place added pressure on the radiologist to rush the interpretation. It also complicates diagnostic evaluation since, even if the diagnostic facility is separate from the screening facility, patients that need to be added on complicate an organized schedule. Although it is inconvenient for the patient, I think it is far safer and more efficient for the screening studies to be read in bulk at a later time in a quiet location at a pace set by the radiologist who has no distractions and not rushed by a stressed waiting room. This means that women will be recalled for additional evaluation, which is inconvenient and anxiety provoking, but is the safest approach. The reason for screening is to detect cancers early, at a curable stage. It is not to provide rapid interpretations to quell some anxiety while missing cancers as a consequence.
[1] Moskowitz M. Screening is Not Diagnosis. Radiology 1979;133:265-267
[2] Kopans DB, Meyer JE, Cohen AM, Wood WC. Palpable breast masses: the importance of preoperative mammography. JAMA 1981; 246:2819-2822.
[3] Wald NJ, Murphy P, Major P, Parkes C, Townsend J, Frost C. UKCCCR multicentre randomized controlled trial of one and two view mammography in breast cancer screening. BMJ 1995; 311:1189-1193.
[4] Baines CJ, Miller AB, Kopans DB, Moskowitz M, Sanders DE, Sickles EA, To T,Wall C. Canadian National Breast Screening Study: assessment of technical quality by external review. AJR Am J Roentgenol. 1990 Oct;155(4):743-7.
[5] Kopans DB. The Canadian Screening Program: A Different Perspective. AJR 1990 155:748-749


