内乳淋巴结
BIRADS 2类的发现
乳腺中有许多病变不是乳腺癌,也不会发展为癌症,比如囊肿和纤维腺瘤。解读乳腺X射线筛查结果的一个重要任务,就是识别出非乳腺癌、不需要召回进行额外评估的病变,其中包括内乳淋巴结。我们曾经在1982年描述了在乳腺X射线摄影图像上发现的内乳淋巴结¹。我不知道有任何胚胎学研究追踪淋巴系统和淋巴结的发育,但由于乳房在上胸壁上发育为一个“皮肤腺”,并且乳房组织通常向上延伸到腋窝,腋窝常见的淋巴结很可能向下延伸到乳房的上部外部,这并不奇怪。
乳腺X射线摄影检查发现,约5%的女性有内乳淋巴结。它们出现在乳腺实质的边缘,靠近皮下脂肪和实质交界处的边缘²。我只见过一个近乳头2/3距离的地方。它们几乎都在乳头的轴线上方。
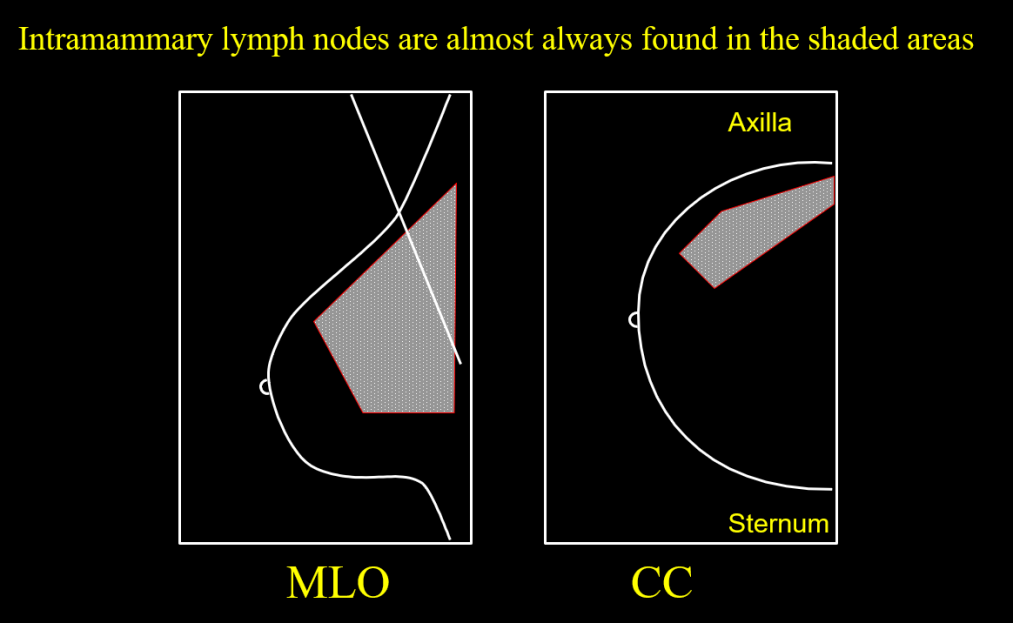
病理学家声称在乳腺的所有象限都发现了淋巴结,但通过乳腺X射线摄影检查发现的淋巴结几乎都在乳腺的侧半部分。据我所知,只有一篇论文报道了两例乳房内侧的内乳淋巴结,但它们被描述为“淋巴组织”,而没有被描述为事实上的“淋巴结”³。
如果在乳房的外侧半部,有一个轮廓清晰的结构,可能略呈分叶状,大小为1厘米或更小,形状为“肾形”,就可以做出安全的诊断。这种形状是由于淋巴结的脂肪脐部,当淋巴结节被“正面”看到时,常常被视为一个放射状的中心。
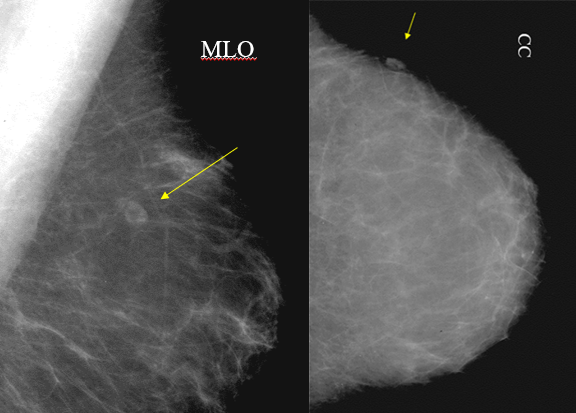
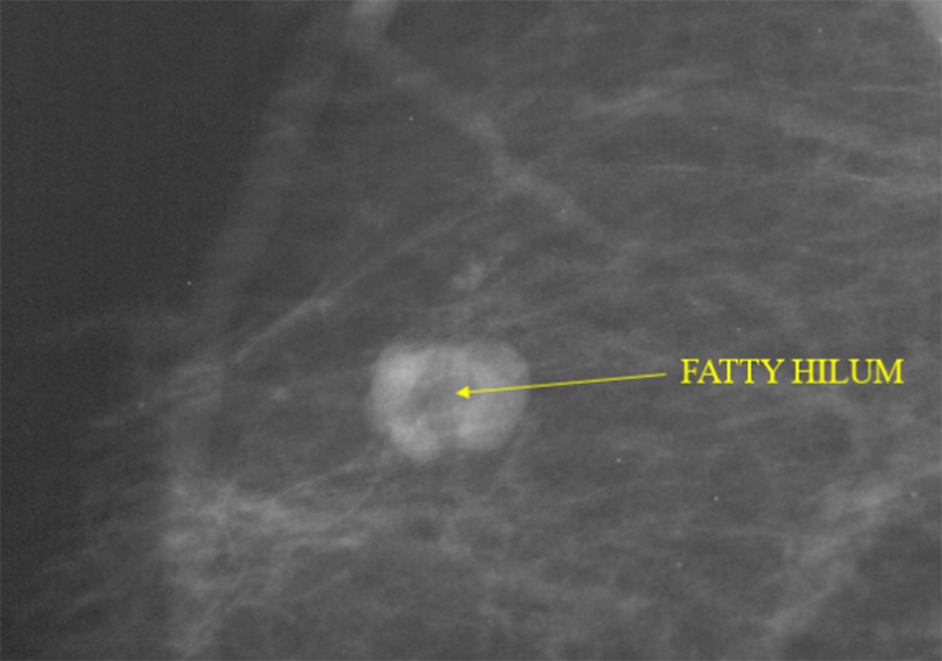
锐利的边缘和肾形是最重要的标准,脐结构内的脂肪进一步增加了确定性。如果存在这些标准,则无需进一步检查。
内乳淋巴结的存在非常普遍,因此可能不需要对其进行BIRADS 2分类,除非担心经验较少的人看到它可能产生误解,而BIRADS 2分类明确澄清其良性性质。
位置的重要性
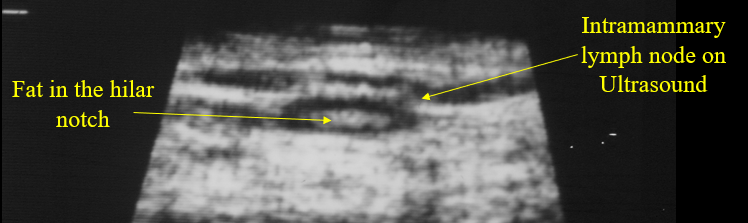
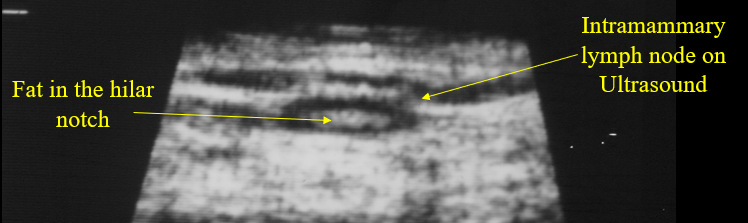
当在乳房的任何其他部分看到肿块时,不应解释为内乳淋巴结,除非病变有明确的透明脐结构。由于并非所有上外象限肿块都是良性淋巴结,如果病变不具备良性内乳淋巴结的形态学特征,包括肾盂形状或透明的脐状切迹以及光滑、轮廓清晰的边缘,则上外象限病变应引起怀疑。如果形态学不清楚,放大的乳腺X射线摄影可以更好地显示形状和清晰的边缘。如果仍然不确定,可以用乳腺超声来显示脐状切迹中的回声脂肪。
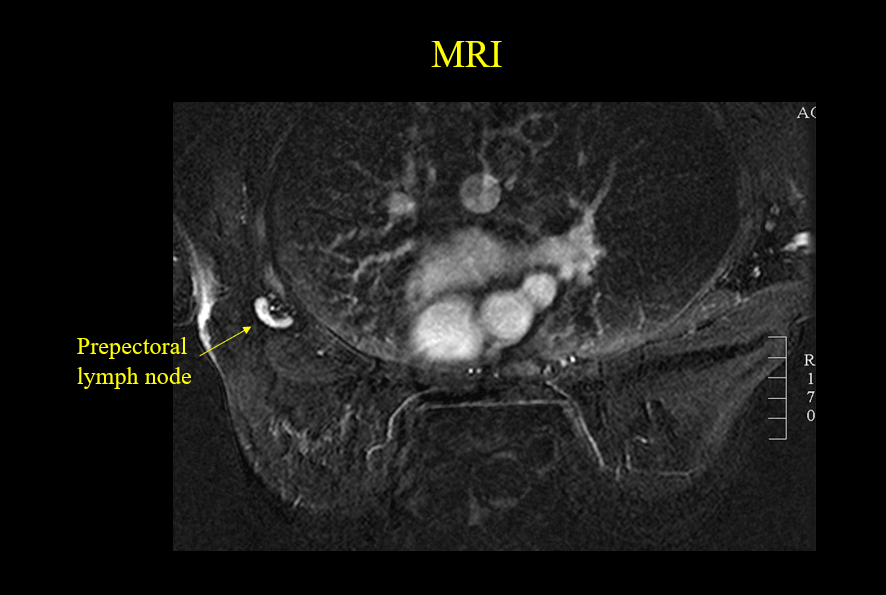
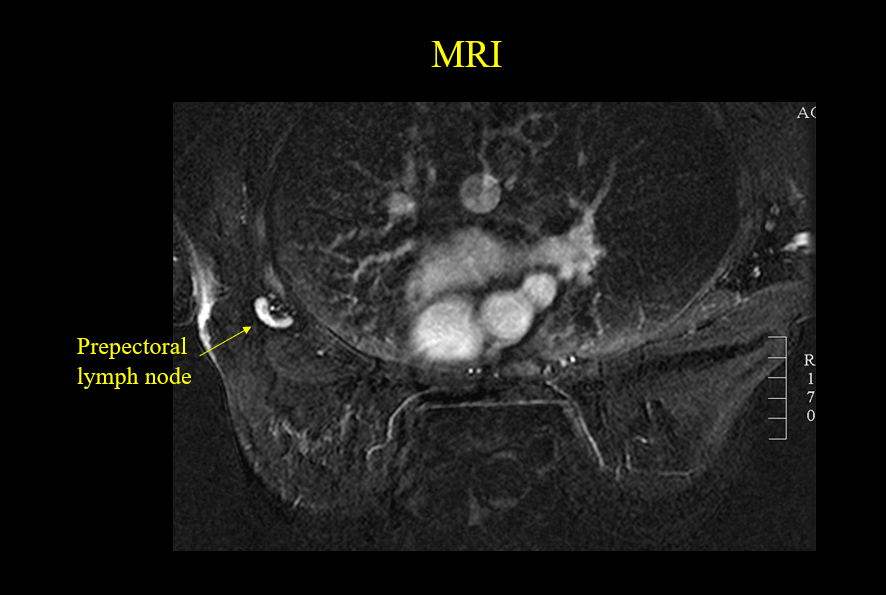
我们也看到过非常少见的乳房深处朝向乳房中心的内乳淋巴结。这些“胸前”淋巴结在乳腺X射线摄影图像上很少见,偶尔在MRI上能看到。
转移到内乳淋巴结的病变
乳腺癌可以扩散到内乳淋巴结。当淋巴结大于1厘米,呈圆形或椭圆形,无脐状结构时,应怀疑内乳淋巴结受恶性病变转移⁴。
我们曾在伴有皮炎或乳腺炎的妇女中看到内乳淋巴结的良性肿大。但如果没有这些明确的淋巴结增大的原因,则建议对1cm或更大、圆形或椭圆形且没有脂肪脐结构的内乳淋巴结进行活检⁶。
对于涉及内乳淋巴结转移性的临床意义似乎仍有一些争论。有些人认为这与有腋窝淋巴结转移是一样的,并预测预后较差⁷,但其也有不同意见⁸⁹¹⁰ 。
乳腺淋巴瘤
原发性淋巴瘤也可累及内乳淋巴结。我们发表了一篇论文,其中包括五位原发性淋巴瘤在乳腺的女性,以及七位已知其他部位淋巴瘤但内乳淋巴结也有受累的女性。异常的乳腺X射线摄影发现的表现有多种:从相当离散的结节到实质和皮肤的弥漫性受累¹¹。
结论
良性的内乳淋巴结很常见。如果它们位于乳房的外边缘(通常位于乳头的轴线上方,直径小于等于1厘米,边缘清晰,呈环状,脐部有脂肪),则无需进一步检查。
中英翻译
BIRADS 2 FINDINGS
There are numerous lesions that develop in the breast that are not breast cancer and do not become cancer such as cysts and fibroadenomas. One of the important aspects of interpreting mammography screening studies is being able to identify findings on the study that do not represent breast cancer and do not need the patient to be recalled for additional evaluation. Among these are intramammary lymph nodes. We described intramammary lymph nodes, found on mammograms, in 1982 ¹. I am not aware of any embryological studies that track the development off the lymphatic system and nodal development, but since the breast develops as a “skin gland” on the upper chest wall, and breast tissue commonly extends up into the axilla, it is it is likely, and not surprising that lymph nodes, commonly seen in the axilla, extend down into the upper outer portion of the breast.
Intramammary lymph nodes are seen, mammographically, in approximately 5% of women. They appear at the edge of the parenchymal cone of the breast, toward the periphery near the junction of the subcutaneous fat and the parenchyma ². I have only seen one that was more than 2/3 of the way to the nipple. They are also almost all above the axis of the nipple.

Pathologists claim to have found lymph nodes in all quadrants of the breast, but the lymph nodes evident by mammography are almost (if not) all in the lateral half of the breast. To my knowledge there has been only one paper that presented two cases of intramammary lymph nodes evident by mammogrpahy in the medial breast, but these were described as “lymphoid tissue” and an actual “node” was not described ³.
The diagnosis is safely made for a structure in the lateral half of the breast toward its periphery that is sharply defined, perhaps slightly lobulated, 1 cm or smaller in size, and “reniform” in shape. This shape is due to the fatty hilum of the node that is often seen as a radiolucent center when the node is seen “en face”.
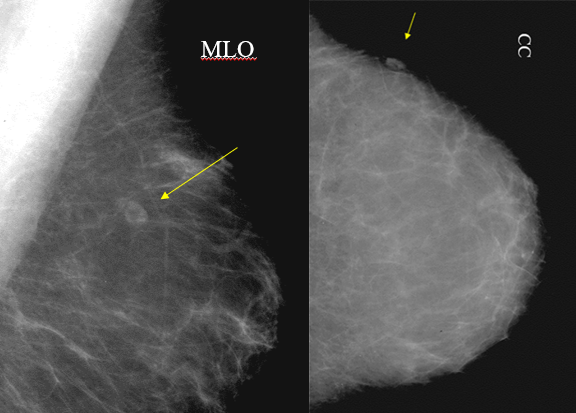
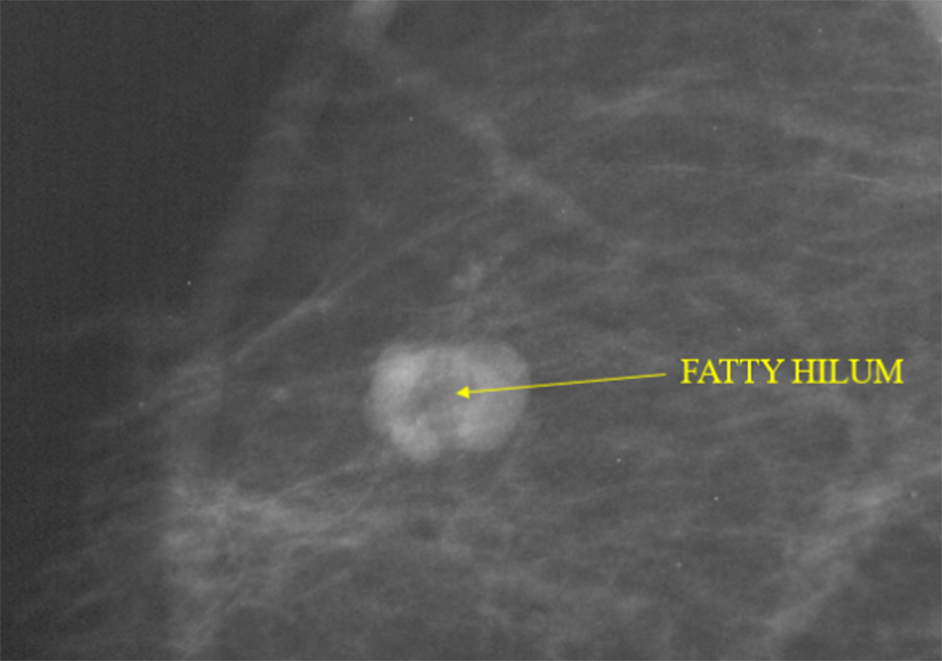
The sharp margins and reniform shape are the most important criteria. Fat in the hilum increases the certainty. When these criteria are present, then no further investigation is needed.
The presence of intramammary lymph nodes is so common, that a BIRADS 2 classification may not be needed unless there is concern that someone with less experience might misinterpret the node and a BIRADS 2 identification will clarify its benign nature.
LOCATION IS IMPORTANT
The interpretation of an intramammary lymph node should not be made when a mass is seen in any other section of the breast unless the lesion has a clearly defined lucent hilum. Since not all upper-outer quadrant masses are benign lymph nodes, if the lesion does not have the morphological characteristics of a benign intramammary lymph node, including a renifrorm shape or a lucent hilar notch and smooth, sharply defined margins, an upper-outer-quadrant lesion should arouse suspicion. If the morphology is not clear, magnification mammography may better demonstrate the shape and sharply defined margins. If this is not convincing, then ultrasound can be used to show the echogenic fat in the hilar notch.
It is very unusual, but we have seen intramammary lymph nodes deep in the breast toward the center of the breast. These “prepectoral” lymph nodes can rarely be seen on mammograms and, on occasion, be seen on MRI.
METASTATIC DISEASE TO AN INTRAMAMMARY LYMPH NODE
Breast cancer can spread to intramammary lymph nodes. Intramammary lymph node involvement should be suspected when the node is larger than 1 cm and is round or oval without a hilum, and there is an associated breast malignancy ⁴.
We have seen benign enlargement of intramammary lymph nodes in women who have an associated dermatitis or mastitis. Without these other clear causes for nodal enlargement, biopsy is recommended for intramammary lymph nodes of 1 cm or greater that are round or oval and do not have a fatty hilum ⁵.
There still seems to be some debate about the clinical significance of metastatic disease involving an intramammary node. Some argue that it is the same as having axillary lymph node involvement ⁶ and predicts a poorer outcome ⁷, but others disagree⁸⁹¹⁰.
LYMPHOMA INVOLVING THE BREAST
Primary lymphoma can also involve intramammary lymph nodes. We published a paper that included five women whose primary lymphoma was in the breast and seven who had known lymphoma elsewhere with lesions in the breast as well. The abnormal mammographic findings varied from fairly discrete nodules to diffuse involvement of the parenchyma and skin¹¹.
CONCLUSIONS
Benign, intramammary lymph nodes are very common. If they are in the outer periphery of the breast (usually above the axis of the nipple, and are 1 cm. or smaller with sharply defined margins and a reinform shape with fat in the hilum, no further investigation is required.
REFERENCES
1.Meyer JE, Kopans DB. The radiographic appearance of normal intramammary lymph nodes. Breast 1982; 40:30-32.
2.Stomper PC, Leibowich 5, Meyer JE. The prevalence and distribution of well circumscribed nodules on screening mammography: analysis of 1500 mammograms. Breast Dis 1991:4:197-203 2. Gordon PB, Gilks B. Sonographic appearance of normal
3.Meyer JE, Ferraro FA, Frenna TH, et al. Mammographic appearance of normal intramammary lymph nodes in an atypical location. AJR Am J Roentgenol 1993;161:779–780
4.Günhan-Bilgen I, Memiş A, Ustün EE. Metastatic intramammary lymph nodes: mammographic and ultrasonographic features. Eur J Radiol. 2001 Oct;40(1):24-9. doi: 10.1016/s0720-048x(01)00373-4. PMID: 11673004.
5.Lindfors KK, Kopans DB, Googe PB, McCarthy KA, Koerner FC, Meyer JE. Breast cancer metastasis to intramammary lymph nodes. AJR Am J Roentgenol. 1986 Jan;146(1):133-6. doi: 10.2214/ajr.146.1.133. Erratum in: AJR Am J Roentgenol 1986 Mar;146(3):614. PMID: 3000154.
6.Lee S, K, Kim S, Choi M, -Y, Kim J, Lee J, Jung S, P, Choe J, -H, Kim J, -H, Kim J, S, Kil W, H, Lee J, E, Nam S, J: The Clinical Meaning of Intramammary Lymph Nodes. Oncology 2013;84:1-5. doi: 10.1159/000340016
7.Hogan BV, Peter MB, Shenoy H, Horgan K, Shaaban A. Intramammary lymph node metastasis predicts poorer survival in breast cancer patients. Surg Oncol. 2010 Mar;19(1):11-6. doi: 10.1016/j.suronc.2008.12.009. Epub 2009 Jan 26. PMID: 19171479.
8.Diaz R, Degnim AC, Boughey JC, Nassar A, Jakub JW. A positive intramammary lymph node does not mandate a complete axillary node dissection. Am J Surg. 2012 Feb;203(2):151-5. doi: 10.1016/j.amjsurg.2011.01.030. Epub 2011 Jul 23. PMID: 21788008.
9.Khoury T, Fang Y, Karabakhtsian R, Mokhtar Desouki M, Nayak A, Hanna M, Sanati S, Peng X, Yan L, Li X, Fadare O, Ambrosone C, Jabbour N, Gaudioso C. The clinical significance of metastatic breast carcinoma to intramammary lymph node. Breast J. 2020 Feb;26(2):197-205. doi: 10.1111/tbj.13636. Epub 2019 Oct 6. PMID: 31588665; PMCID: PMC7869654.
10.Guth AA, Mercado C, Roses DF, Hiotis K, Skinner K, Diflo T, Cangiarella J. Intramammary lymph nodes and breast cancer: a marker for disease severity, or just another lymph node? Am J Surg. 2006 Oct;192(4):502-5. doi: 10.1016/j.amjsurg.2006.05.011. PMID: 16978960.
11.Meyer JE, Kopans DB, Long JC. Mammographic appearance of malignant lymphoma of the breast. Radiology. 1980 Jun;135(3):623-6. doi: 10.1148/radiology.135.3.7384445. PMID: 7384445.


