PREOPERATIVE MAMMOGRAPHICALLY GUIDED LOCALIZATION (2)
ONCE THE LOCALIZATION IS COMPLETE DO NOT BEND THE WIRE TO SECURE IT
If the tip of the needle had been about 1 cm. beyond the lesion; and if the bend in the hook had been just inside the tip of the needle; and if the wire had been held firmly while the needle was withdrawn over the wire; the hook should have opened just beyond the lesion with the lesion centered on the thick segment of the wire just proximal to the hook. The last image to obtain is the view perpendicular to the course of the wire after the needle has been withdrawn that, ideally, shows the lesion with the wire through it (or alongside – some lesions cannot be penetrated) and the lesion on the thickened segment with the hook just beyond the lesion.
The thick segment is a marker for the surgeon so that when she/he is dissecting down the wire, and reaches the thick segment, they know that the lesion is next and they can excise the volume of tissue containing the thick segment, the hook, and the lesion.
There is no reason to return to the projection looking down the wire. The needle had already been passed through or alongside the lesion and since the tip of the needle is never pulled back proximal to the lesion the wire will be in the same position that the needle had been so there is no need to confirm its relationship to the lesion. In fact, unless there was some problem, DO NOT return to the first projection and DO NOT COMPRESS THE BREAST IN THE DIRECTION THAT THE WIRE IS PASSING since this will risk displacing the wire potentially advancing the hook deeper.
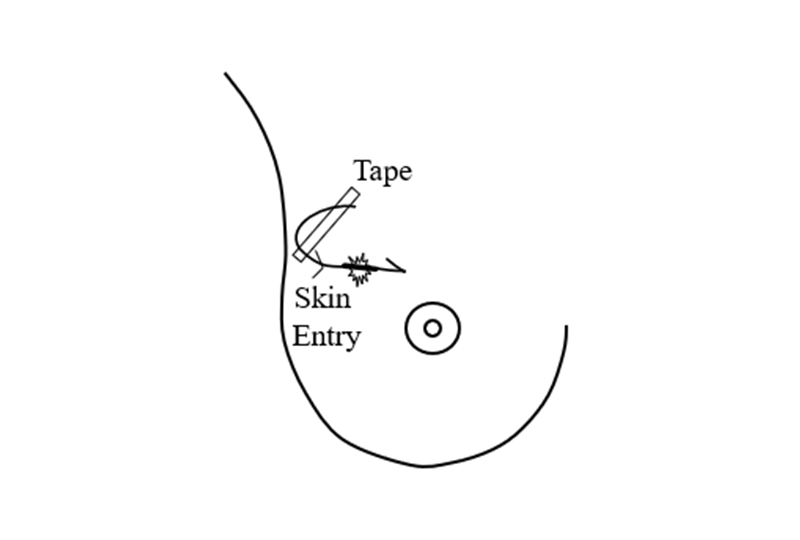
Once the hook, the wire, and their relationship to the lesion is established, the patient is removed from compression and the breast is allowed to relax on the chest wall. The wire may appear to move further into the breast or move out as the breast re-expands. This is not a problem since, if the wire is not under tension, the hook will maintain its relationship just beyond the lesion. It is a mistake to bend the wire or tape it tightly to the skin since this might pull the hook out of the lesion as the breast moves. The wire should be gently looped on the chest and taped with no tension,and covered with a sterile pad.
The patient can then proceed to the operating room.
SURGICAL BIOPSY
Because the wire is always positioned parallel to the chest wall using mammographic techniques, it is virtually impossible to cause a pneumothorax, a risk and a reason to not perform “freehand” localizations. With accurate localization we have found that the surgery can almost always be performed safely in an outpatient setting using local anesthesia making the entire process very safe.
It is a good idea to help the surgeon by sending a diagram, such as the one below, to the operating room with the patient.
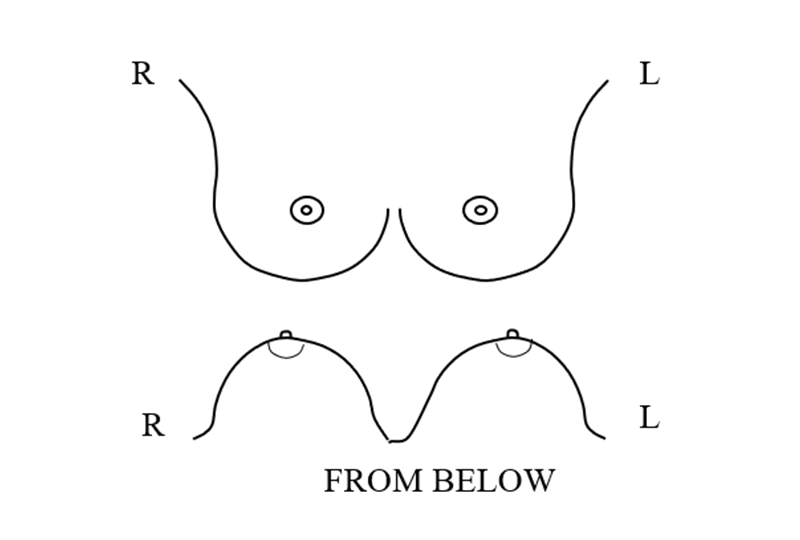
The radiologist draws on the diagrams to show the surgeon the location of the lesion in the breast and the relationship of the wire to the lesion.
Although the surgeon will see the patient in the operating room in the supine position with the breast flattened out on the chest, the diagram provides the surgeon an indications as to the relationship of the skin entry point; the wire; the course of course of the wire; and location of the lesion in the breast and on the wire. The location of the lesion, and the course of the wire should be as accurate as possible so that the surgeon can plan the most direct route to the lesion to produce the best cosmetic result with the removal of just the amount of tissue needed as in the example below.
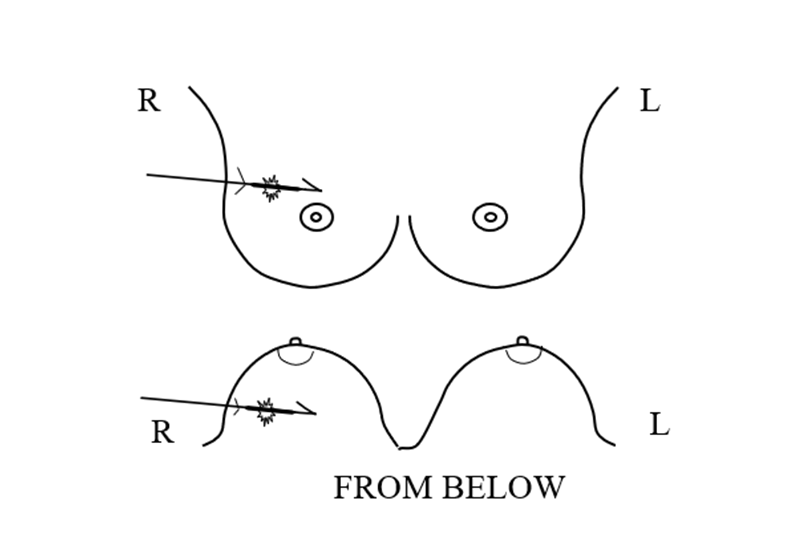
Often the best surgical approach is for the surgeon to follow the wire into the breast from the skin insertion. However, if the lesion is deep and toward the center of the breast and if the wire takes a long course inside the breast to the lesion, using the diagrams as a guide, the surgeon may want to make the skin incision further along the course of the wire to shorten the dissection to the lesion.
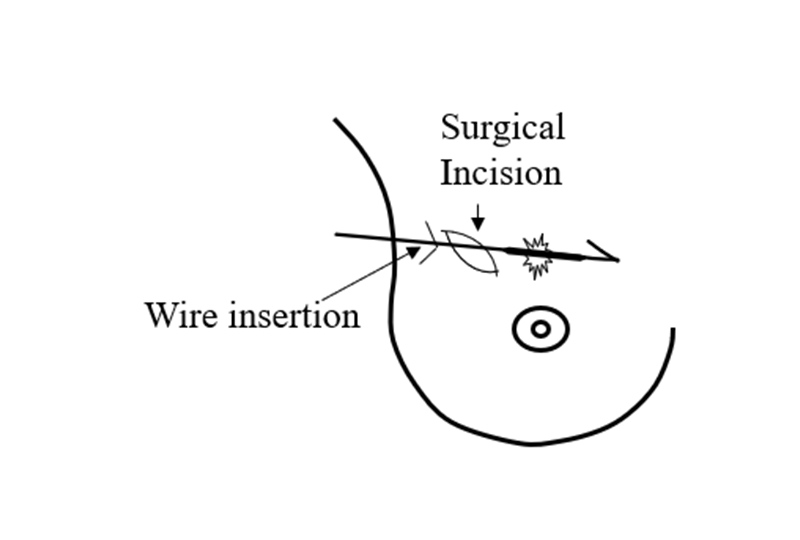
Dissecting down to the wire, the surgeon then dissects along the wire to the thick segment and removes the tissue down and around the thick segment and the hook to remove the tissue containing the lesion.
SPECIMEN RADIOGRAPHY
Before the surgery is concluded a specimen radiograph should be obtained. It is important that the surgeon either return the excised tissue to the Breast Imaging Division or have a specimen radiography unit in the operating room that can, ideally, send the image, digitally, to the radiologist that performed the localization so that she/he can confirm that the lesion has been excised. Confirmation is critical since cancers have been missed when this is not done.
The excised tissue should be gently compressed. Too much compression can alter the relationship of the lesion to the excised tissue margins, but, without some compression, air may be trapped in the specimen obscuring the details of the tissues.
Since specimen radiography is generally a two-dimensional image, it is not possible to determine if the margin of the excised lesion is free of involvement if the targeted lesion is malignant. However, if the radiographically visible lesion abuts a margin on the radiograph, then margin involvement is almost certain. If there is obvious involvement of the lesion at the margin of the specimen on the specimen radiograph, then the surgeon may wish to remove additional tissue along the walls of the excision. Some surgeons do this routinely calling them “shaved margins”.
POST OPERATIVE CONCORDANCE
It is critical that the radiologist confirm that the radiographically visible lesion has been excised but checking for concordance does not end with the specimen radiograph. It is important that the pathologist confirm, if calcifications were the targeted lesion, that the pathological review identifies the calcifications seen on the mammogram. What most don’t realize is that the pathologist only reviews very small samples of the excised tissue even if the removed tissue includes a relatively small volume. For pathological review the excised tissue is cut into 2 mm. thick sections and then these are embedded into paraffin and 5 micron shavings are made from the top of the “block”. It would take 2000 slides to review the entire block and there are often multiple blocks. Although, on a statistical level, and with random slices, it is likely that the lesion gets evaluated, it is important to realize that the pathologists is definitely not able to evaluate the lesion in its entirety.
It is not unusual for the targeted lesion to be deeper in the block than the top 5 micron planes so that it is possible that the pathologist might not see the histology of the targeted lesion. If there is any question, the paraffin blocks should be returned to Breast Imaging and x-rays taken with the blocks held on their side so that if the calcifications are deeper in the block, their depth in the block can be determined so the pathologist can obtain “levels” through the block.
In addition, it is important to remember that when the pathologist determines that the margins of the excised tissues are “clear”, meaning that there is no tumor visible at the margin, this is a “best guess”. This supports the hope that the lesion has been completely removed and if malignant there is no residual tumor in the breast. Again, although this is the best we can do at this time, it is not particularly accurate. If we could be certain that there is no residual cancer in the breast, then radiation would not be needed, but since we are unable to be completely confident, post operative treatment is often needed. Remember, because the excised tissue is cut into sections, and only a few 5 micron slices of each is evaluated, most of the “margin” of the excised tissue is not actually evaluated. Statistically the random sampling is fairly accurate, but it is impossible to determine whether or not a cancer has been completely removed.


