乳腺X射线摄影引导下的术前定位(二)
定位完成后,不要弯曲钩丝进行固定
理想的钩丝定位流程:针尖在病灶外大约1cm的位置,钩丝末端弯曲部分刚好在针尖内,退出针鞘后,钩丝牢牢钩住腺体组织,钩丝加粗部分位于病灶中心,钩丝末端刚好在病灶以外打开。最后,退出针鞘后,我们要拍一张与钩丝呈垂直方向的图像。正常情况下,图像上应该显示钩丝穿过病灶(或旁边,如果一些病灶无法穿透),钩丝加粗部分位于病灶内,末端在病灶外。
钩丝加粗部分是帮助外科医生识别的一个标记,当他们沿着钩丝切入到了加粗部分时,就会知道下面是病灶,这样他们就可以将钩丝加粗部分,末端部分和病灶组织一起切除了。
我们不需要再次拍片去确认钩丝位置。当针已经穿过病灶或在病灶周边,钩丝末端在针尖位置,那么针鞘退出后,钩丝末端就在病灶近端,我们不需要再去确认它的位置。事实上,除非有什么问题,否则不需要在第一个投照角度再次拍摄,也不要在钩丝穿过病灶的方向压迫乳房,因为这将有可能使钩丝移位,钩尖进入到更深的位置。
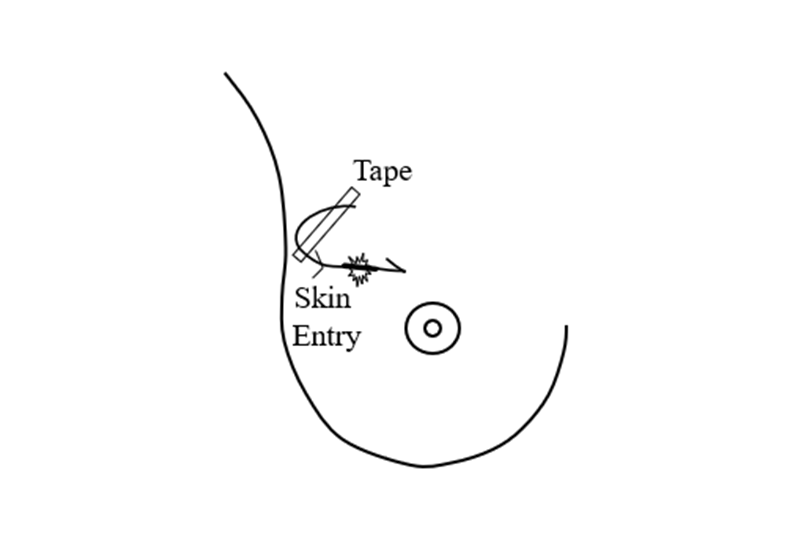
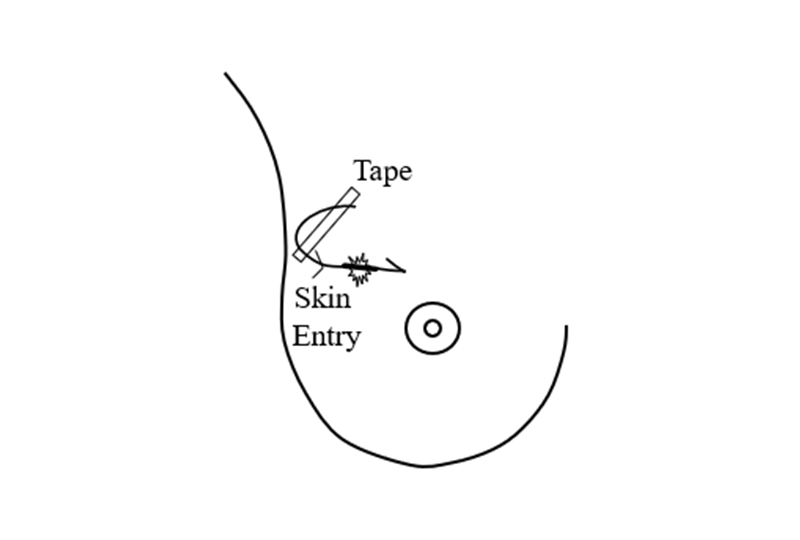
只要确定了钩丝,弯曲的末端与病灶位置,就可以释放对于患者的乳房压迫,使乳房在胸壁上处于放松状态。随着乳房因压迫释放而变大的时候,钩丝可能会进一步向乳房内或外移动。但这并不影响什么,只要金属钩丝不在绷紧状态,钩丝就会固定在病灶位置上保持不变。将钩丝弯曲或紧贴在皮肤上是错误的,因为这可能导致乳房移动,钩丝从病灶处脱出。 应将钩丝轻轻地绕在胸前,并用胶带将其固定,注意不要让它有张力,再用无菌垫覆盖。然后病人就可以进手术室了。
手术活检
在使用乳腺X射线摄影进行穿刺引导时,钩丝走向应始终与胸壁保持平行,这样就基本可以避免引起气胸,这也是不进行“徒手”穿刺定位的原因。我们发现在门诊局麻下通过术前精准定位引导手术非常安全。
还有一个可以更好帮助外科医生的建议,就是画一张示意图(如下图),和病人一起送到手术室。
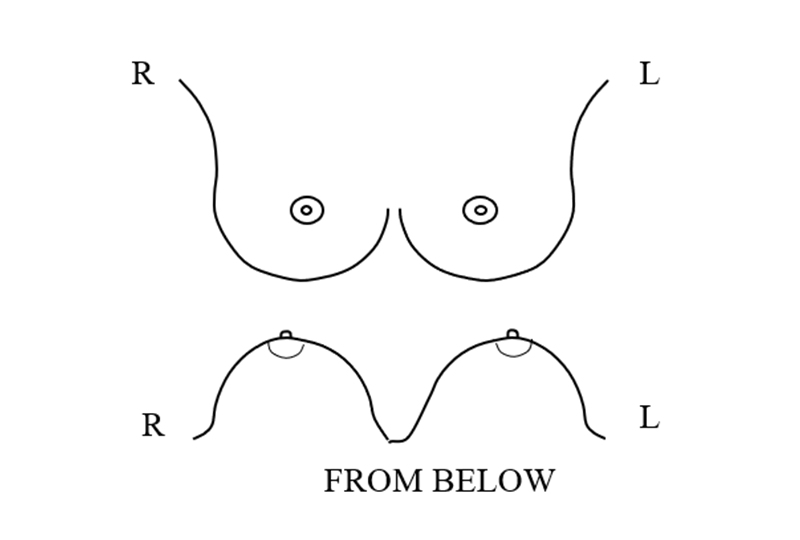
放射科医生通过画出的示意图,明确告诉外科医生病变位置以及钩丝与病灶的位置关系。
虽然患者在手术室为仰卧位,乳房平铺在胸壁上,但外科医生可以根据这张图看到病灶和钩丝的位置,钩丝走行与皮肤切口的相互关系。病灶的位置和钩丝的走向应尽可能准确,以便外科医生能够规划出最短手术路径,只切除必要的乳腺组织,以达到最佳的美观效果,如下例所示。
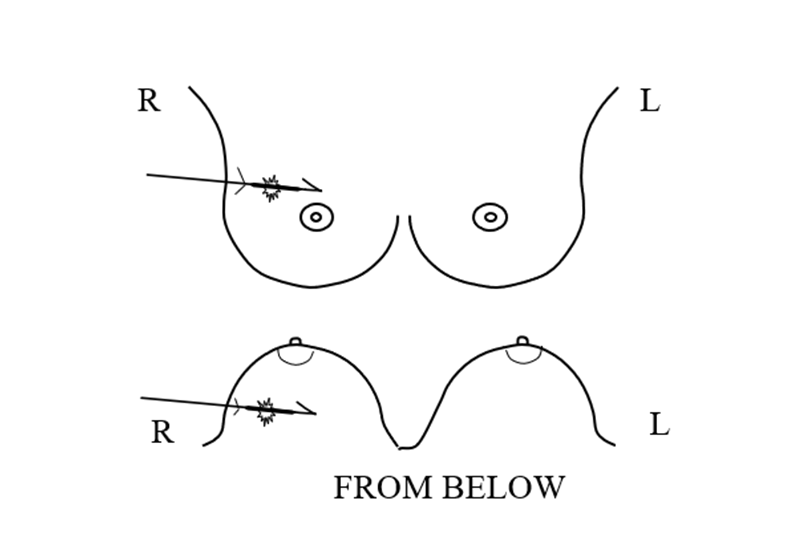
通常情况下,最好的手术方法是外科医生从皮肤切口处沿着钩丝进入乳房。但是,如果病灶位置比较深或位于乳房中间,乳房内钩丝到病灶处的距离比较长,如下图所示,外科医生就可能会在钩丝路径方向再做一个切口,以缩短切除病灶的手术路径。
然后,外科医生沿着钩丝,切除钩丝加粗部分至钩丝末端周围含病灶的组织。
标本摄影
在手术结束前,应该做一个标本摄影。外科医生可以将切除的组织送到放射科或者在手术室配备专门的标本拍摄系统。最好能将数字图像发送给负责定位的放射科医生来确认病灶已经切除。这个确认的步骤非常重要,否则容易漏掉癌症。
切下的组织要轻轻压迫,压力过大的话会改变病灶与切除组织边缘的关系。但是不压迫也不行,因为如果没有一定的压迫,标本组织中的细节可能会被潴留期中的空气所掩盖。
标本摄影通常是二维图像,如果是恶性病灶,就没有办法确认已经切除的病灶边缘是否累及。但是如果在X射线图像上看到了病灶与切缘相毗邻,那么基本可以确定切缘累及。如果标本X光片上的切缘有明显的病灶累及,外科医生就需要沿着切缘切除更多的额外组织。
术后的一致性
至关重要的是,放射科医生要确认X光片上可见的病变已被切除,但仅通过标本影像检查一致性还不够。病理学的确认也很重要。如果钙化是目标病变,要在病理切片时找到在乳腺X射线摄影图像上看到的钙化。大多数人没有意识到的是,病理科医生只审查非常少量的切除组织样本,即使切除的组织体积很小。病理检查时,切除的组织会被切成2毫米厚的切片,嵌入石蜡中形成蜡块儿,然后再将蜡块制作成5um的切片。一个蜡块可能会被切成2000片,而且还经常有多个蜡块标本。虽然,在统计水平上,随机查看切片基本上可以对病灶进行评估,但是重要的是,我们要知道,病理科医生绝对不可能对整个病灶进行评估。
目标病灶在蜡块中的位置低于顶部的5微米厚层并不罕见,因此病理科医生就有可能看不到病灶的组织学信息。如果有任何的疑问,应该将石蜡块送回乳腺影像科并将其侧放拍摄X光片,这样,如果钙化在石蜡块中位置比较深,就可确定它在蜡块内的深度,以便病理科医生了解其在蜡块内的“层面”。
此外,重要的是要记住,当病理学家确定切除组织的边缘是“干净”的,也就是说在边缘没有看到肿瘤,这只是一种“最佳猜测”。这支持了人们的希望,即病变已被完全切除,如果是恶性的,则乳房中没有残留的肿瘤。同样,尽管这是我们目前能做的最好的结果,但它并不是特别准确。如果我们能够确定乳房中没有残余的癌症,那么就不需要进行放射治疗,但由于我们无法完全确定,所以往往需要进行术后治疗。请记住,由于切除的组织被切成不同的部分,每个部分只有几个5微米的切片被评估,大部分切除的组织的“边缘”实际上没有被评估。从统计学上看,随机抽样是相当准确的,但不可能完全确定癌症是否被完全切除。
中英翻译
ONCE THE LOCALIZATION IS COMPLETE DO NOT BEND THE WIRE TO SECURE IT
If the tip of the needle had been about 1 cm. beyond the lesion; and if the bend in the hook had been just inside the tip of the needle; and if the wire had been held firmly while the needle was withdrawn over the wire; the hook should have opened just beyond the lesion with the lesion centered on the thick segment of the wire just proximal to the hook. The last image to obtain is the view perpendicular to the course of the wire after the needle has been withdrawn that, ideally, shows the lesion with the wire through it (or alongside – some lesions cannot be penetrated) and the lesion on the thickened segment with the hook just beyond the lesion.
The thick segment is a marker for the surgeon so that when she/he is dissecting down the wire, and reaches the thick segment, they know that the lesion is next and they can excise the volume of tissue containing the thick segment, the hook, and the lesion.
There is no reason to return to the projection looking down the wire. The needle had already been passed through or alongside the lesion and since the tip of the needle is never pulled back proximal to the lesion the wire will be in the same position that the needle had been so there is no need to confirm its relationship to the lesion. In fact, unless there was some problem, DO NOT return to the first projection and DO NOT COMPRESS THE BREAST IN THE DIRECTION THAT THE WIRE IS PASSING since this will risk displacing the wire potentially advancing the hook deeper.
Once the hook, the wire, and their relationship to the lesion is established, the patient is removed from compression and the breast is allowed to relax on the chest wall. The wire may appear to move further into the breast or move out as the breast re-expands. This is not a problem since, if the wire is not under tension, the hook will maintain its relationship just beyond the lesion. It is a mistake to bend the wire or tape it tightly to the skin since this might pull the hook out of the lesion as the breast moves. The wire should be gently looped on the chest and taped with no tension,and covered with a sterile pad.
The patient can then proceed to the operating room.
SURGICAL BIOPSY
Because the wire is always positioned parallel to the chest wall using mammographic techniques, it is virtually impossible to cause a pneumothorax, a risk and a reason to not perform “freehand” localizations. With accurate localization we have found that the surgery can almost always be performed safely in an outpatient setting using local anesthesia making the entire process very safe.
It is a good idea to help the surgeon by sending a diagram, such as the one below, to the operating room with the patient.
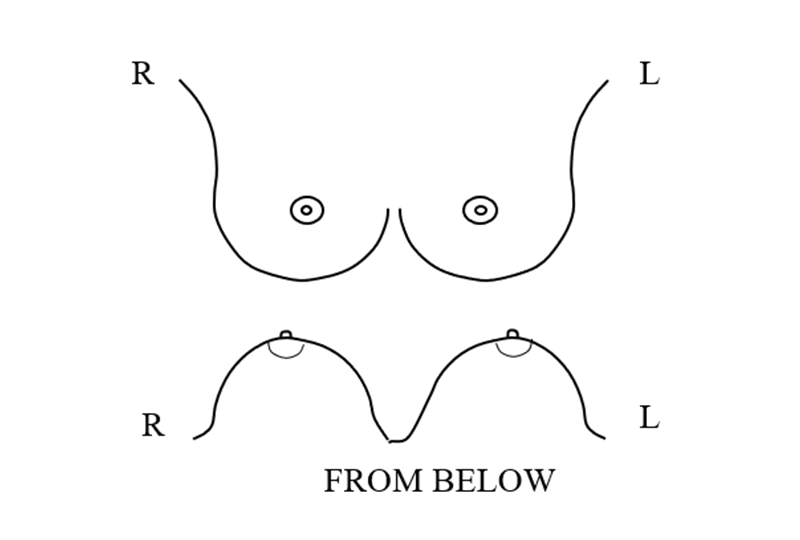
The radiologist draws on the diagrams to show the surgeon the location of the lesion in the breast and the relationship of the wire to the lesion.
Although the surgeon will see the patient in the operating room in the supine position with the breast flattened out on the chest, the diagram provides the surgeon an indications as to the relationship of the skin entry point; the wire; the course of course of the wire; and location of the lesion in the breast and on the wire. The location of the lesion, and the course of the wire should be as accurate as possible so that the surgeon can plan the most direct route to the lesion to produce the best cosmetic result with the removal of just the amount of tissue needed as in the example below.
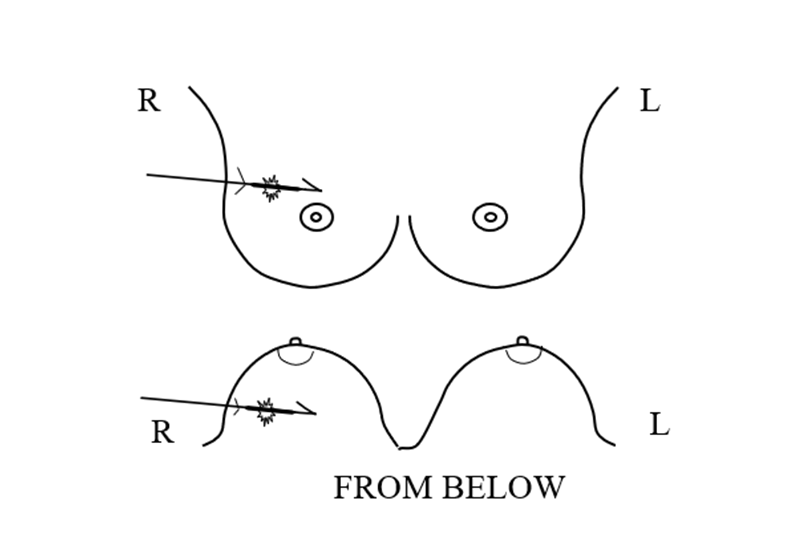
Often the best surgical approach is for the surgeon to follow the wire into the breast from the skin insertion. However, if the lesion is deep and toward the center of the breast and if the wire takes a long course inside the breast to the lesion, using the diagrams as a guide, the surgeon may want to make the skin incision further along the course of the wire to shorten the dissection to the lesion.
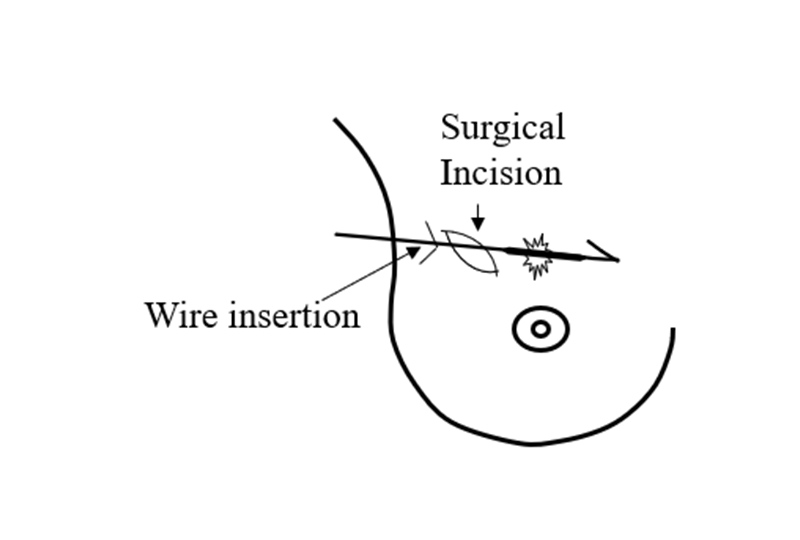
Dissecting down to the wire, the surgeon then dissects along the wire to the thick segment and removes the tissue down and around the thick segment and the hook to remove the tissue containing the lesion.
SPECIMEN RADIOGRAPHY
Before the surgery is concluded a specimen radiograph should be obtained. It is important that the surgeon either return the excised tissue to the Breast Imaging Division or have a specimen radiography unit in the operating room that can, ideally, send the image, digitally, to the radiologist that performed the localization so that she/he can confirm that the lesion has been excised. Confirmation is critical since cancers have been missed when this is not done.
The excised tissue should be gently compressed. Too much compression can alter the relationship of the lesion to the excised tissue margins, but, without some compression, air may be trapped in the specimen obscuring the details of the tissues.
Since specimen radiography is generally a two-dimensional image, it is not possible to determine if the margin of the excised lesion is free of involvement if the targeted lesion is malignant. However, if the radiographically visible lesion abuts a margin on the radiograph, then margin involvement is almost certain. If there is obvious involvement of the lesion at the margin of the specimen on the specimen radiograph, then the surgeon may wish to remove additional tissue along the walls of the excision. Some surgeons do this routinely calling them “shaved margins”.
POST OPERATIVE CONCORDANCE
It is critical that the radiologist confirm that the radiographically visible lesion has been excised but checking for concordance does not end with the specimen radiograph. It is important that the pathologist confirm, if calcifications were the targeted lesion, that the pathological review identifies the calcifications seen on the mammogram. What most don’t realize is that the pathologist only reviews very small samples of the excised tissue even if the removed tissue includes a relatively small volume. For pathological review the excised tissue is cut into 2 mm. thick sections and then these are embedded into paraffin and 5 micron shavings are made from the top of the “block”. It would take 2000 slides to review the entire block and there are often multiple blocks. Although, on a statistical level, and with random slices, it is likely that the lesion gets evaluated, it is important to realize that the pathologists is definitely not able to evaluate the lesion in its entirety.
It is not unusual for the targeted lesion to be deeper in the block than the top 5 micron planes so that it is possible that the pathologist might not see the histology of the targeted lesion. If there is any question, the paraffin blocks should be returned to Breast Imaging and x-rays taken with the blocks held on their side so that if the calcifications are deeper in the block, their depth in the block can be determined so the pathologist can obtain “levels” through the block.
In addition, it is important to remember that when the pathologist determines that the margins of the excised tissues are “clear”, meaning that there is no tumor visible at the margin, this is a “best guess”. This supports the hope that the lesion has been completely removed and if malignant there is no residual tumor in the breast. Again, although this is the best we can do at this time, it is not particularly accurate. If we could be certain that there is no residual cancer in the breast, then radiation would not be needed, but since we are unable to be completely confident, post operative treatment is often needed. Remember, because the excised tissue is cut into sections, and only a few 5 micron slices of each is evaluated, most of the “margin” of the excised tissue is not actually evaluated. Statistically the random sampling is fairly accurate, but it is impossible to determine whether or not a cancer has been completely removed.


